 In Clinical Infectious Diseases Elin Svensson and colleagues showed that increasing rifampicin exposure shortened the time needed to reach undetectable levels of bacteria in sputum. The effect did not plateau within the studied range of exposures, indicating that doses higher than 35 mg/kg could be yet more effective.
In Clinical Infectious Diseases Elin Svensson and colleagues showed that increasing rifampicin exposure shortened the time needed to reach undetectable levels of bacteria in sputum. The effect did not plateau within the studied range of exposures, indicating that doses higher than 35 mg/kg could be yet more effective.
Background. Tuberculosis remains a huge public health problem and the prolonged treatment duration obstructs effective tuberculosis control. Higher rifampicin doses have been associated with better bactericidal activity, but optimal dosing is uncertain. This analysis aimed to characterize the relationship between rifampicin plasma exposure and treatment response over 6 months in a recent study investigating the potential for treatment shortening with high-dose rifampicin.
Methods. Data were analyzed from 336 patients with pulmonary tuberculosis (97 with pharmacokinetic data) treated with rifampicin doses of 10, 20, or 35 mg/kg. The response measure was time to stable sputum culture conversion (TSCC). We derived individual exposure metrics with a previously developed population pharmacokinetic model of rifampicin. TSCC was modeled using a parametric time-to-event approach, and a sequential exposure-response analysis was performed.
Results. Higher rifampicin exposures increased the probability of early culture conversion. No maximal limit of the effect was detected within the observed range. The expected proportion of patients with stable culture conversion on liquid medium at week 8 was predicted to increase from 39% (95% confidence interval, 37%–41%) to 55% (49%–61%), with the rifampicin area under the curve increasing from 20 to 175 mg/L·h (representative for 10 and 35 mg/kg, respectively). Other predictors of TSCC were baseline bacterial load, proportion of culture results unavailable, and substitution of ethambutol for either moxifloxacin or SQ109.
Conclusions. Increasing rifampicin exposure shortened TSCC, and the effect did not plateau, indicating that doses >35 mg/kg could be yet more effective. Optimizing rifampicin dosage while preventing toxicity is a clinical priority.
Publication
The Potential for Treatment Shortening With Higher Rifampicin Doses: Relating Drug Exposure to Treatment Response in Patients With Pulmonary Tuberculosis.
Svensson EM, Svensson RJ, Te Brake LHM, Boeree MJ, Heinrich N, Konsten S, Churchyard G, Dawson R, Diacon AH, Kibiki GS, Minja LT, Ntingiya NE, Sanne I, Gillespie SH, Hoelscher M, Phillips PPJ, Simonsson USH, Aarnoutse R.
Elin Svensson , Rob Aarnoutse , Lindsey te Brake and Martin Boeree are members of theme Infectious diseases and global health.
-
Want to know more about these subjects? Click on the buttons below for more news.
Related news items

David Burger top scientist on anti-HIV medication
6 December 2021 Professor of Clinical Pharmacy David Burger, affiliated with the Radboudumc Pharmacy, is in the list of top scientists in the field of anti-HIV medication. read more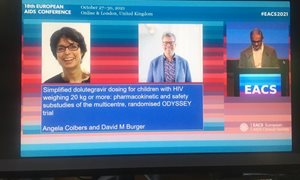
The European Hector Research Award in HIV 2021 awarded to Angela Colbers and David Burger
2 November 2021 On Friday 29 October 2021, during the 18th European AIDS Conference in London, the Hector Research Award for the best scientific article related to clinical or epidemiological HIV research was presented to Angela Colbers and David Burger, both working in the Pharmacy of the RadboudUMC. read more
Anti-tuberculosis drug can be safely dosed even higher
16 March 2021 A considerably higher dose of the anti-tuberculosis drug rifampicin is safe and can also lead to a shorter treatment for tuberculosis and less resistance. read more
Rob Aarnoutse is appointed as professor in Translation pharmacology of antimicrobial agents in particular drugs for tuberculosis
25 January 2021Hospital pharmacist and clinical pharmacologist Rob Aarnoutse is appointed as professor in ‘Translation pharmacology of antimicrobial agents, in particular drugs for tuberculosis’ at Radboud University / Radboudumc, starting 16 November 2020.
read more
Radboudumc research leads to simplified dose of HIV medication for children
31 August 2020 For children living with HIV, an adapted, simpler combination therapy is now available. Thanks to research by the Radboudumc, it is now clear that the use of one easily available tablet of dolutegravir in children gives just as good treatment results as a combination of several. read more
